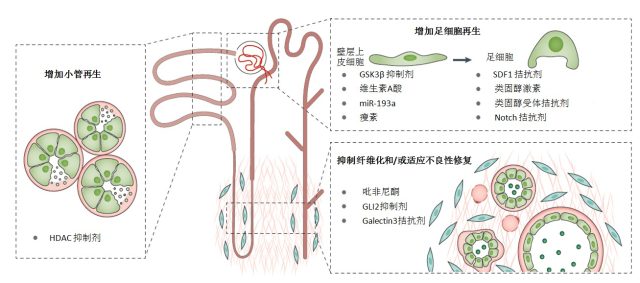
Hip fracture is the plain English term for a proximal femoral fracture or PFF. It refers to a fracture occurring in the area between the edge of the femoral head and 5 centimetres below the lesser trochanter (Figure 1). These fractures are generally divided into two main groups depending on their relationship to the capsule of the hip joint. Those above the insertion of the capsule are termed intracapsular, subcapital or femoral neck fractures. Those below the insertion are extracapsular. The extracapsular group is split further into trochanteric (inter- or pertrochanteric and reverse oblique) and subtrochanteric as shown. The division into intra and extracapsular fractures relates to both the blood supply of the femoral head and the mechanics of fixation.
Hip fracture is a major public health issue due to an ever increasing ageing population. About 70,000 to 75,000 hip fractures (proximal femoral fractures) occur annually in the UK, with a cost (including medical and social care) amounting to about £2 billion a year. Demographic projections indicate that the UK annual incidence will rise to 91,500 by 2015 and 101,000 in 202039, with an associated increase in annual expenditure. The majority of this expenditure will be accounted for by hospital bed days and a further substantial contribution will come from health and social aftercare. At present about a quarter of patients with hip fracture are admitted from institutional care, and about 10–20% of those admitted from home ultimately move to institutional care.
Hip fracture is the commonest reason for admission to an orthopaedic trauma ward and is usually a ‘fragility’ fracture1 caused by a fall affecting an older person with osteoporosis or osteopaenia (a condition in which bones lose calcium and become thinner, but not as much as in osteoporosis). The National Hip Fracture Database reports the average age of a person with hip fracture as 84 years for men and 83 for women, 76% of fracture occur in women. Mortality is high – about 10% of people with a hip fracture die within 1 month and about one third within 12 months. Most of the deaths are due to associated co morbidities and not just to the fracture itself reflecting the high prevalence of comorbidity in people with hip fracture. It is often the occurrence of a fall and fracture that signals underlying ill health. Thus, hip fracture is by no means an exclusively surgical concern. Its effective management requires the co-ordinated application of medical, surgical, anaesthetic and multidisciplinary rehabilitation skills and a comprehensive approach covering the full time course of the condition from presentation to subsequent follow-up, including the transition from hospital to community.
Although hip fracture is predominantly a phenomenon of later life, it may occur at any age in people with osteoporosis or osteopenia, and this guidance is applicable to adults across the age spectrum. Skills in its management have, however been accrued, researched and reported especially by collaborative teams specialising in the care of older people (using the general designation ‘orthogeriatrics’). These skills are applicable in hip fracture irrespective of age, and the guidance includes recommendations that cover the needs of younger patients by drawing on such skills in an organised manner.
This guidance covers the management of hip fracture from the point of admission to secondary care through to final return to the community and discharge from specific follow-up. It assumes that anyone clinically suspected of having a hip fracture will be referred for immediate hospital assessment other than in exceptional circumstances. It excludes (other than by cross-reference) aspects covered by parallel NICE guidance, most notably primary and secondary prevention of fragility fractures, but recognises the importance of effective linkage to these closely related elements of comprehensive care.
The diagnosis of hip fracture is easily missed and in a small minority of patients the fracture may not be apparent on a plain X-ray. In view of the serious nature of hip fracture the guidance has sought to identify the most cost-effective imaging strategies to ensure this does not happen.
Although not a structured service delivery evaluation, the Guideline Group was required to extend its remit to cover essential implications for service organisation within the NHS where these are fundamental to hip fracture management, and this has been done. In general it is the case that suboptimal care and/or fragmentation of care result in longer periods of dependency and/or hospitalisation leading to greater cost as well as inferior outcome. There is substantial variation and lack of clarity in the UK in the extent, timing, manner and organisation of the necessary collaborative and multidisciplinary elements of effective management, including the timely achievement of rehabilitation after surgery according to individual need. A further concern is the occurrence of delay before necessary
surgery is carried out. Prompt surgery has been generally recognised to be important, but surgery is sometimes delayed for administrative or clinical reasons. Emerging evidence from the National Hip Fracture database indicates substantial variation across centres in England and Wales in this and other indicators of clinical and service quality. Such variation has potentially profound economic implications, and priority has been given where appropriate to underpinning recommendations with any available evidence of cost-effectiveness in the NHS. Since work began on the guideline the Department of Health in England has launched a high priority Best Practice Tariff initiative targeting a range of performance variables for hip fracture, and the GDG have been aware of this contextual change as well as of humanitarian issues in evaluating the evidence and formulating recommendations.
At all stages of hip fracture management, the importance of optimal communication with, and support for, patients themselves and those who provide or will provide care – including unpaid care family members or others – has been a fundamental tenet of guidance development.
The view of the GDG is that an exceptional contemporary window of opportunity exists in the NHS to achieve major improvements in the delivery of hip fracture care, to the benefit not only of patients but of the system as a whole in terms of efficiency and cost. It is hoped that implementation of this guidance will be instrumental to that end.
髋部骨折 2011年英国国家临床攻略中心成人髋部骨折治疗攻略
精彩推荐
- 突破十万交付大关!全新问界M7用硬核实力回应市场认可

在风起云涌的新能源汽车市场,一款车型能否成为真正的标杆,往往并不只取决于华丽的技术参数或前卫的设计语言,而在于它能否真正走进千家万户,赢得用户用选择投出的信任票...详细
- 光影与智慧的双重献礼:解析尊界S800如何借新春OTA重塑豪华出行

在智能汽车不断刷新功能边界的今天,一次真正有意义的OTA升级,应如春风化雨,既能雕琢体验的细微之处,亦能筑牢安全的钢铁长城。岁序更迭,万象更新之际,尊界S800奉上精...详细
- 智能革命,豪华新生!尊界S800以双重价值重塑百万座驾标杆

长久以来,百万级豪华车市场犹如一个被精心守护的俱乐部。然而,一款来自中国的座驾尊界S800,正以破竹之势改写规则。它不仅连续五个月稳坐70万元以上细分市场销冠,更以五...详细
- 问界新M5 Ultra破解冬季出行痛点,至高享37000元限时礼遇

寒冬时节,对于每一位车主而言,都是一场对车辆性能与舒适性的严峻考验。冰冷的座椅、缓慢的充电效率、湿滑难行的道路,这些熟悉的冬季限定痛点,不仅影响着出行体验,更关...详细
本周热门
- 同仁堂健康双十一活动开启 “象食养医”倡导从健康的时候就关注健康
如果你想了解自己身体的秘密,让健康成为日常的生活方式,保持年轻的状态,实现抗衰老,逆生长的美好愿望,那么今年双十一的这场活动你一定不要错过。11月1日,同仁堂健康...详细